Ebola: ‘We Are Ready’
While the first cases of Ebola in the United States have sparked nationwide concern, the overwhelming message here on the South Fork is that health care providers are prepared to handle patients with Ebola-like symptoms, just as they handle other infectious diseases.
“We’re taking it seriously, as it should be,” said Dr. Maury Greenberg, a doctor at East Hampton Urgent Care, of the largest Ebola outbreak in history.
The first case diagnosed in the U.S. took the life of a Liberian man who was being treated at a Dallas hospital two weeks ago. Two nurses who treated him were diagnosed soon after. The condition of one was upgraded to “good” on Tuesday; the other is reported to be improving as well.
All others who had contact with the man, either outside or inside the hospital, have so far tested negative for the disease, which has primarily been contained to West Africa. Still, there have been several scares in the tri-state area. A Yale University student who had just returned from Liberia came down with symptoms earlier this month and was quarantined; she has now tested negative for Ebola. A Liberian national who arrived at Newark Airport in New Jersey via Brussels with a fever on Tuesday was reported “asymptomatic” late yesterday.
Following instructions from the Centers for Disease Control, health care facilities and emergency medical service providers are implementing procedures. The New York State Department of Health issued emergency health orders on Monday.
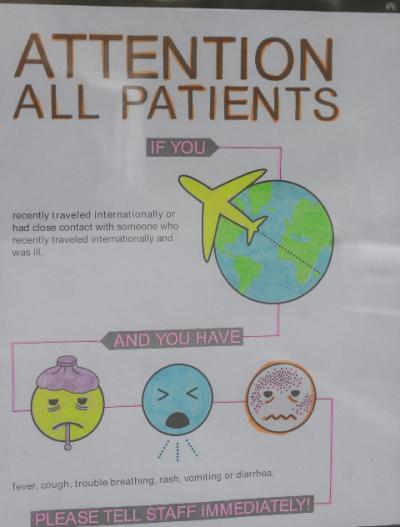
Southampton Hospital, Wainscott Walk-In, East Hampton Urgent Care, and other providers have signs on the doors alerting patients that if they have been traveling and have certain symptoms, to take a mask, cover their faces, and immediately alert the front desk.
Ebola spreads through direct contact with bodily fluids, and a cough could infect a person who is sprayed with saliva. Symptoms such as headache, fever, and aches, begin 8 to 10 days after exposure, and can appear as late as 21 days later, according to the C.D.C. A rash, diarrhea, and vomiting may also occur. Severe cases may cause hemorrhage.
Although health care providers are at the highest risk of getting sick, many here are said to be taking the threat of exposure in stride and using it as a reminder to always be vigilant. “It’s a generic awareness — it’s not just Ebola,” Dr. Greenberg said. “If somebody comes in with a fever, stiff neck, and muscle pains, they could have meningitis. Someone coming in with a weird rash could be chicken pox or measles. Measles is more contagious than Ebola. There’s a lot of health
concerns out here.”
“We’ve got everybody getting masks out there right now — there’s so much going on outside of Ebola,” said Kate Skinner, the practice manager at Wainscott Walk-In. “So much depends on the patient doing the right thing. I definitely see people are reading the sign.”
Diane O’Donnell, chief of the East Hampton Village Volunteer Ambulance Association, has taken steps to ensure her crew knows what precautions to take. Next week, she and two other association members will take a class in leadership awareness offered by Suffolk County, and bring back the information. “This is a good opportunity to make sure that everything we are doing is safe,” said Ms. O’Donnell. “It is a good reminder to people not to get complacent. You really don’t know what is out there.”
Ms. O’Donnell, a critical care technician who has volunteered for the past 10 years, cited incidents of exposure to other infectious diseases, such as tuberculosis, bacterial meningitis, and respiratory viruses, that gave cause for just as much concern. “People have always been adequately protected,” she said.
To ensure E.M.S. providers wear the proper personal protective equipment, including gowns, goggles, and face masks, when responding to a call, dispatchers throughout the county have been trained to ask callers specific questions related to Ebola. The East Hampton Village Emergency Communications Department, which dispatches five of the six fire and ambulance districts as well as two of the three police departments that serve the Town of East Hampton, implemented new procedures on Friday.
Village Police Chief Gerard Larsen, who oversees the department, said public safety dispatchers will now ask whether a caller has traveled in the last few weeks — the incubation period — or has been around anyone who has traveled, and will screen for symptoms, such as an elevated temperature. Police and E.M.S. providers will then be notified, if necessary, that they are responding to a “fever-travel” call.
The Southampton Village Communications Department, which dispatches the Bridgehampton Fire Department, will act similarly, using the phrase “I.D. response,” for infectious disease.
East Hampton Town and Village police have been directed to respond to, but not go into, a house or business where a patient with such symptoms is located. If they have to go in, they must don a biochemical suit covering every part of the body.
“We are prepared — that’s the most important message to get out there,” said Marsha Kenny, the director of public affairs and relations at Southampton Hospital. Anyone exhibiting symptoms, whether walking into the lobby or arriving by ambulance, will be put in an isolation area in the emergency department and treated as if they have the disease. A blood sample will be taken and sent for review; results come back within 24 hours. Confirmed Ebola patients will be transported to Stony Brook University Hospital, which is the designated regional hospital.
Dr. Darin G. Wiggins, the head of the hospital’s emergency department, Dr. Fredric I. Weinbaum, chief medical officer, and Deborah Maile R.N., director of infection prevention, have met on a regular basis. “We’ve been at this probably over two weeks now,” Ms. Kenny said, adding that all the necessary gear was ordered at the start of the scare, in anticipation that it would be in high demand.
Employees have been trained one-on-one in the use of personal protective equipment. Those receiving training include those in registration and “environmental services,” or housekeeping. “They are on the front lines too,” Ms. Kenny said. “These hazmat-trained security people are also repeating the training, just to make sure that employees who have to wear this clothing are very confident in their skills in getting dressed up and dressed down.” Practice drills are being scheduled, she said.
